What Does the FDA’s Ethylene Oxide Medical Device Sterilization Program Mean for You?
The Food and Drug Administration (FDA) has recently addressed the need for more innovation in medical device sterilization techniques. It has selected 11 participants to help develop new methods in this field.
Many patients rely on effective medical device sterilization to ensure that their devices are safe for use. The FDA’s push for improved medical device sterilization systems highlights the agency’s focus on improving patient outcomes and the quality of care and service that they provide.
The new pilot program will test ethylene oxide sterilization methods for medical devices to see if any improvements can be made.
What Methods of Sterilization Are Being Used Now?
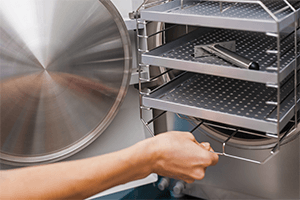
A variety of methods are currently in use for medical device sterilization:
- Dry heat
- Radiation
- Steam
- Vaporized hydrogen peroxide
- Nitrogen dioxide
- Vaporized peracetic acid
- Chlorine dioxide gas
- Ethylene oxide
These options all come with limitations, as many of them risk damaging the medical equipment in the process and may leave dangerous residues behind. For example, steam sterilization is unsuitable for sensitive electronics.
FDA Seeks to Improve Ethylene Oxide Sterilization
On November 25, 2019, the FDA launched a master pilot program involving the chemical ethylene oxide.
The program, titled, the Ethylene Oxide Sterilization Master File Pilot Program (EtO Pilot Program), is a voluntary initiative that aims to streamline the process for sterilization providers and device manufacturers. The program aims to make changes between sterilization sites and modify processes that use reduced EtO concentrations.
Ethylene oxide is a widely-used method of sterilization that is unlikely to damage medical equipment, which is why an estimated 50% of all medical devices in the United States use this method.
Two voluntary consensus standards apply to ethylene oxide sterilization:
The FDA’s Planned Changes
The FDA’s main objectives are to identify new sterilization methods and technologies and to reduce ethylene oxide emissions. To that end:
- New safety standards will regulate how much ethylene chlorohydrin residue is allowed to exist after the sterilization process.
- Service providers will also need to submit a PMA supplement to the FDA for review to determine whether they meet international standards.
- Inspections will ensure that industrial facilities engaged in sterilization and state health departments for health care facilities using ethylene oxide are up to standard.
- The FDA recommends 510(k) holders review the guidance document: “Deciding When to Submit a 510(k) for a Change to an Existing Device.”
Ensure That Your Organization Is Meeting Medical Device Best Practices
The FDA is seeking to develop, validate, and control sterilization for medical devices in support of their patient-first initiatives.
Because of these changes, it is vital that you report any adverse changes that result from the FDA’s new efforts. These types of changes may require additional medical device training courses, certifications, and the submission of updated documentation.
We recommend you check out the following medical device training courses and certifications:
- Intro to Medical Device Submission - 510(k)s, PMAs & Exemptions
- (CMWP) Certified Medical Writing Professional
- Preparation of FDA Submissions and Communicating with the FDA
Keep your medical device protocols up to date with streamlined pharmaceutical training courses offered by the Center for Professional Innovation and Education. You can get in touch with a member of our team by calling 1-610-648-7550 or emailing info@cfpie.com.
Blog Categories
Stay Informed